Infertility and the anaesthetist
The decision of if, and when, to start a family can be a difficult one for a medical
professional trying to balance training, exams and career progression. Having
made such a decision, there is a natural expectation that the pitter-patter of little
feet will follow shortly. However, for a not insignificant proportion of couples,
infertility and baby loss is a real and unspoken issue.
My motivation for writing this article is twofold:
- anaesthetists are involved in many stages of the
fertility journey. From anaesthetising for initial
investigations to egg collections and surgical
management of miscarriage (SMM). By increasing
understanding, I hope that this will encourage us to
provide supportive and empathic care during these
highly anxious and emotional experiences.
- with increased focus on wellbeing, I thought that it
was time to raise awareness of the issue in order
to improve understanding, and support those of us
who are struggling.
Fertility statistics
The NHS website reports that while 84% of couples will
conceive within a year of having unprotected sex, around one
in seven will have problems conceiving [1]. While many may be
struggling with infertility, I believe that it is rarely discussed. No
doubt, speaking to one’s colleagues about one’s sex life is not
usual work chat. The very real feeling of failure inevitably plays
a part.
Following a period of trying to conceive naturally, the usual
next step is to pursue medical investigations, followed by
intervention. There are many treatments options available; one
in particular, often perceived as a ‘quick fix’, is in vitro fertilisation (IVF). There are many detailed variations of IVF, but three
common themes are:
- it is a long and trying journey, both physically and
emotionally.
- NHS funding is limited and hard to obtain (only 35% of
cases [2]), and the costs are significant for those paying
privately.
- success rates are much lower than general perceptions;
29% of under-35s having a life birth after embryo transfer,
decreasing to 9% for age 40-42 [2].
While medical professionals have a vague understanding of the
concept of IVF, one often overlooked aspect is the significant
amount of time required for attending appointments. During
ovarian stimulation, daily scans and bloods may be required
for a period of up to 14 days. For many professions, especially
medics, taking a few hours out of the working day can prove
challenging.
Baby loss
Infertility is a very broad topic and doesn’t just encompass not
being able to conceive – baby loss is a significant challenge
in and of itself, with one in four pregnancies ending in loss
during pregnancy or birth [3]. The fact that it is so common
should not detract from the physical and emotional effects
of losing a pregnancy. It is a sad reality that, as anaesthetists,
we far too regularly encounter baby loss in our working lives,
with a constant trickle of 'SMMs' booked onto the emergency
list. Have we become de-sensitised to this loss? With losses
occurring before the pregnancy announcement, many couples
will suffer in silence.
The psychological aspect
We must not underestimate the emotional demands that
infertility and baby loss have on a person. The physical impact
of treatments would normally last for a matter of months.
The feeling of loss, failure and inadequacy is much longer
lasting. One study suggested that the psychological symptoms
of infertility are comparable to those with serious medical
conditions such as cancer [4]. Insecurities and self-doubt in
one’s personal life can creep into the workplace. It can be
difficult to watch colleagues fall pregnant and have babies.
Labour ward placements may prove to be particularly difficult.
The fact that there is little openness and discussion around this
topic compounds the issue.
Being now aware of the prevalence of infertility, let’s turn to the
support available:
The formal NHS employers leave policy is
‘There is no statutory
entitlement to time off for IVF or other fertility treatment’
[5].
Whilst IVF and related treatments are elective, it is somewhat
surprising that there is such a lack of formal support available
from our employer, after all infertility is a recognised medical
condition. This seems somewhat short sighted from the
perspective of supporting staff wellbeing.
For late baby loss, leave is in line with the typical employer
maternity policy. However, for baby loss up to week 25, only
normal sickness provisions apply. This can leave staff feeling
pressured to return to work.
Practical advice
Speaking from a trainee perspective, I would strongly encourage
you to chat with your College Tutor, or a consultant that you trust,
as it is likely that they have supported other trainees through
similar circumstances and may well be more knowledgeable
than you expect. They may be able to link you to a peer for
support. Getting to know the rota co-ordinator can be helpful in
maximising training opportunities, whilst balancing treatment
demands. It is important to highlight that the departments that
I have worked in have been supportive and accommodating,
and gone beyond that permitted by the NHS guidelines; for that
I am incredibly grateful. My comments here are from a female’s
perspective, but I hope that in the future someone is able to
provide a male’s (or other denomination’s) perspective.
Advice to supporting colleagues
Be supportive. Be approachable. Be kind. Alice Rose, an infertility
commentator, runs a campaign of what not to say to those
affected [6]. This includes “you can just adopt/do IVF”, “just relax”,
“at least you know you can get pregnant”, “just stop trying and it’ll
happen” or “go on holiday”.
All pregnancies are precious, but those after loss or infertility
come with a lot more anxiety and apprehension. Not working
nights during treatment or pregnancy should not be viewed as
laziness.
My story
I am in my higher stage of anaesthesia training in London. I (well, my husband and I – it is a couple’s journey!) were lucky to
get pregnant naturally in 2018. I was naturally anxious, but took
reassurance from a heartbeat scan at eight and ten weeks. The
13-week scan was less hopeful: a strong heartbeat, but a fetal
abnormality was detected. After an excruciating two weeks of
waiting and extensive testing, we made the difficult decision
to end the pregnancy. Fast forward two years, and after two
investigative operations and multiple fertility treatments including
IVF, we are no closer to bringing that much wanted baby home.
I have chosen to remain anonymous. We are still working through
our fertility journey, and for now we would like it to remain private.
For me, my work is my escape; it is an immersive place where I
do not have to discuss fertility. However, I am more than happy
to chat individually about my experiences, or support anyone struggling with fertility, as I know what a lonely place it can be.
My email is
[email protected] (Instagram
@thelonghardroad), and I promise that anything talked about will
be in the strictest confidence.
Resources
There are many support groups and resources available, in
particular a confidential support group for medical staff having
IVF (Box 1).
A London Higher Anaesthetics Trainee
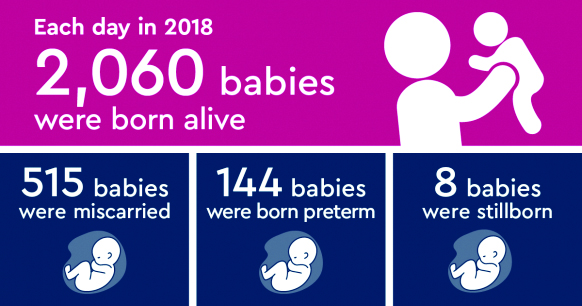
Figure 1 - see [3]
References
- NHS. Overview: infertility, 2020. https://www.nhs.uk/conditions/infertility/
(accessed 2/7/2020).
- Human Fertilisation & Embryology Authority. Choose a fertility clinic,
2019. https://www.hfea.gov.uk/choose-a-clinic/ (accessed 2/7/2020).
- Tommy’s. Pregnancy loss statistics, 2020. https://www.tommys.org/ourorganisation/
our-research/pregnancy-loss-statistics (accessed 2/7/2020).
- Domar AD, Zuttermeister PC, Friedman R. The psychological impact
of infertility: a comparison with patients with other medical conditions.
Journal of Psychosomatic Obstetrics and Gynaecology 1993; 14: S45-52.
- NHS Employers. Guidance on dealing with requests for time off, 2014.
https://www.nhsemployers.org/-/media/Employers/Documents/Pay-andreward/
Guidance-on-time-off-requests-28-Jan.pdf (accessed 2/7/2020).
- Alice Rose. Think! What not to say: to fertility patients, 2020.
https://www.thisisalicerose.com/what-not-to-say (accessed 2/7/2020)